The University of Iowa Department of Orthopedics and Rehabilitation has implemented an orthopedics skills training course for second-year resident physicians. Formed in 2021, this intensive, weeklong simulation-based training program prepares trainees to take on the added responsibilities required of third-year residents, covering training and assessments on level-appropriate skill topics such as joint arthroplasty, upper and lower extremity trauma, arthroscopy, and wire navigation.
“During their third year, residents often take on more responsibilities and gain more autonomy in surgical procedures, so this program helps prepare them for this transition,” says professor and orthopedic surgeon Matthew Karam, MD.
This program comes after the success of the department’s monthlong surgical skills training program for first-year residents. Spearheaded at Iowa in 2013, the program has since become the gold standard and the model for
many other teaching institutions. This training program introduces early-stage orthopedic residents to the skills they will need to be successful surgeons.
“Giving our residents hands-on, focused education and training to develop their surgical skills has been shown to be one of the best ways to prepare them for the rest of their residency,” says Karam, who serves as director of the residency program. “It allows faculty members to provide personalized feedback to guide the residents in their development.”
With the success of the first-year resident training program, Karam was inspired to find a way to prepare orthopedics trainees for the next pivotal moment in their residency: the transition from second to third year.
Building the PGY2 skills course
To plan out the weeklong program, residency program leaders enlisted a
multidisciplinary team of orthopedic surgeons, simulation engineers, and lab administrators who met over the course of six months to develop a curriculum based on subspecialties that are increasingly important to mid-level residents, such as taking care of trauma patients and performing joint arthroplasty procedures.
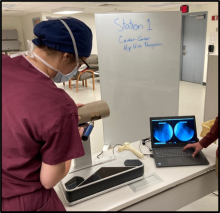
The week is designed with two-and-a-half days devoted to joint arthroplasty training; a half-day for arthroscopy simulation evaluation and procedural training on upper extremity procedures; one day for lower extremity trauma; and a final day focusing on assessments of technical proficiency.
This program’s use of simulators of orthopedic surgery skills allows residents to practice in a safe environment and builds on more than a decade of UI research on the subject. Just recently, Iowa researchers successfully renewed a five-year grant from the Agency for Healthcare Research and Quality to continue their work toward establishing simulation-based training and objective, surgical skill evaluation as a standard part of orthopedic residency training.
During the assessment day, residents rotate through stations, including four simulation stations, and extremity cadaveric stations. Residents also are evaluated on a procedural checklist and an OP-score—the global rating scale recently endorsed by the American Board of Orthopedic Surgeons as a new standard of competency evaluation for residents. Wire navigation skills were assessed by total time, number of fluoroscopy images, and pin placement.
Performance levels were then compared to previously established proficiency benchmarks to identify areas where additional training is needed. Residents also completed a survey regarding the format, training, feedback, and overall effectiveness of the skills week.
Positive results
Following the skills week, each resident was provided a scorecard with their individual data. Assessments showed that for carpal tunnel, distal radius ORIF, and IMN for tibia fracture, residents had achieved level-appropriate metrics using OP-scores. While half of all residents achieved the proficiency benchmark for wire navigation, some residents needed additional practice.
“The implementation of a surgical skills course for PGY2 allowed these residents the ability to focus on more advanced tasks during an important transition in residency training,” says J. Lawrence Marsh, MD, professor and chair of the UI Department of Orthopedics and Rehabilitation. “Our second-year residents found the entire week to be extremely helpful and said they felt much more confident going into their third year of residency.”
Not only have the residents universally given high marks to this new program, but faculty have also been eager to engage and contribute to the ongoing development of the program. While improvements to the week will continue to be made, this program represents the next logical advancement in simulation and skills training for orthopedic residents and provides a framework for other institutions considering a mid-level skills assessment of proficiency. Marsh and Karam hope programs like this one can help better assess residents' skill levels to appropriately structure future training and assessments and help prepare them for the year to come.