Researchers from Iowa's Department of Orthopedics and Rehabilitation have been awarded a five-year, $1.9 million grant from the Agency for Healthcare Research and Quality (AHRQ) to continue their work toward establishing simulation-based training and objective, surgical skill evaluation as a standard part of orthopedic residency training.
The team, led by faculty members Don Anderson, PhD, and Matthew Karam, MD, along with Geb Thomas, PhD, professor in the UI College of Engineering, and researchers from other major universities, aims to explore how simulation-based training programs and prompt, informative performance feedback can be used to reduce errors and increase efficiency for orthopedic residents during surgery.
While simulation-based training and standard competency tests are required in many surgical disciplines, this is not the case for orthopedics.
“Orthopedic residents are supervised by more experienced surgeons in the operating room, but this longstanding training model is being reevaluated, because the operating room is a difficult place to learn certain skills,” Anderson says. “Training orthopedic surgical residents in this way can take years, cost hundreds of thousands of dollars, and potentially compromise patient safety.”
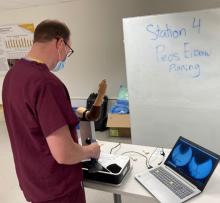
The Iowa research team aimed to improve this process by developing proven simulators like the Core Requisites for Orthopedic Wire Navigation Skills (CROWNS) simulator—a sophisticated, but portable, orthopedic surgery simulator that uses small cameras and synthetic bones to mimic surgery and provide residents with immediate feedback.
After investing in simulation research like what is being done by the Iowa team, the American Board of Orthopaedic Surgery (ABOS) met earlier this spring to discuss their findings. Positive discussions from that meeting led the ABOS to host a Surgical Simulation Summit this past September to consider plans to integrate competency assessment into orthopedic residency programs. “This unprecedented integration will work toward the goal of eventually incorporating simulation-based training as a means of determining competency,” Karam says.
Despite growing interest, ABOS has stopped short of mandating simulation-based training due to insufficient evidence that it improved surgical performance. The research sponsored by this grant may help supply the evidence ABOS needs to advance simulation as a tool for skills training and standardized surgical competency.
“At this stage, we need to be able to scientifically assess if a resident’s ability to perform a surgical procedure has improved as a result of his or her time working with the simulator,” Thomas says. “This involves studying fluoroscopic images to determine the accuracy of the wire placement and then comparing residents who took part in our training with those who have not. With this information, we will have a good idea if our simulator is improving performance.”
The AHRQ project plans to build on the Iowa team’s more than a decade of research on the subject to incorporate more rigorous operating room performance assessment into residency programs. Researchers will continue partnering with ABOS as they work toward improving patient safety through simulation and competency-based training.